Xuanping Zhang and colleagues from the CDC have just published an interesting paper on the prevalence of undiagnosed diabetes. Using data from NHANES (a nationally representative survey), they found that adults without insurance are more likely to have undiagnosed diabetes than those with insurance. Being uninsured for more than a year was associated with 2.5-fold increased risk of having diabetes without a dignosis.
The main message, of course, is that we need much broader (dare I say "universal?") health coverage so we can intervene early and prevent the nasty complications of diabetes. However, Charlie MacLean (my nearly silent partner) brought up an interesting issue: What about insured patients? How often do we miss them? Can we use the laboratory registry to find folks with incidental blood sugar results that warrant a diagnostic work-up?
There are (at least) a few problems: What thresholds should we use? Probably 126 mg/dl for fasting and 200 mg/dl for non-fasting samples to start. Eventually, we could probably work out the risk of diabetes at lower levels of glucose.
How many are there? Damon Lease, our colleague who has done quality management at a small community hospital guestimates that he finds a few dozen a month. A regional registry might find many, many!
Whom should we notify? A blood sugar ordered as part of a chemistry profile in, say, the ER, might get overlooked in the hurly-burly of that setting. The best person to judge its significance and orchestrate follow-up is the Primary Care Provider. However, figuring out who the PCP is from administrative data (and even an EHR) is fraught with difficulty.
So, there are some challenges, but we may be able to take a bite out of the missed diabetes problem.
Ben
The Missed Patient With Diabetes: How access to health care affects the
detection of diabetes
Xuanping Zhang, Linda S. Geiss, Yiling J. Cheng, Gloria L. Beckles, Edward
W. Gregg, and Henry S. Kahn
Diabetes Care 2008;31 1748-1753
http://care.diabetesjournals.org/cgi/content/abstract/31/9/1748?etoc
A personal look at clinical decision support -- using individual information (lab test results, clinical findings, prescriptions, administrative data, etc.) to engage patients, improve individual care, enhance population health, and make health care safer, faster, cheaper and more effective.
Thursday, August 28, 2008
Wednesday, August 27, 2008
Is Vermedx® "Health Information Exchange?"
First, what is "Health Information Exchange?"
“The movement of health-related data–clinical and/or administrative –according to an agreed-upon set of interoperable standards, processes and activities across independently operating organizations in a manner that protects the privacy and security of an individual’s information.” (“Consensus Conventions for the Use of Key HIT Terms” Project – ONC/HHS, 2008)
Well, let's see:
But it is open for business now.Thousands of patients are getting reminders and alerts when their diabetes needs attention. Hundreds of PCPs are getting decision support and advice tailored to their patients' current clinical situation.
I'm very excited about RHIOs and the wonderful potential to make wholesale changes in broad chunks of health care. But, I'm also impatient to start making things better now. So, I'm glad that providers and insurers in my part of Vermont are using Vermedx® to start bringing the information age to us today, while the state-wide infrastructure for a fully-functional RHIO gets put together.
“The movement of health-related data–clinical and/or administrative –according to an agreed-upon set of interoperable standards, processes and activities across independently operating organizations in a manner that protects the privacy and security of an individual’s information.” (“Consensus Conventions for the Use of Key HIT Terms” Project – ONC/HHS, 2008)
Well, let's see:
- move health-related data (mostly clinical) - check
- agreed-upon interoperable standards (among the various labs and practices) - check
- independently operating organizations (dozens of labs, hundreds of practices, few of them even talking to one another, let alone operating together) - check
- privacy and security - check
But it is open for business now.Thousands of patients are getting reminders and alerts when their diabetes needs attention. Hundreds of PCPs are getting decision support and advice tailored to their patients' current clinical situation.
I'm very excited about RHIOs and the wonderful potential to make wholesale changes in broad chunks of health care. But, I'm also impatient to start making things better now. So, I'm glad that providers and insurers in my part of Vermont are using Vermedx® to start bringing the information age to us today, while the state-wide infrastructure for a fully-functional RHIO gets put together.
Tuesday, August 26, 2008
Diabetes Maps for Public Health
Here is an example of what you can do once you have the registry up and running. These data are a few years old, but they show the variation in average A1C across a large swath of New England and upstate New York.

Many of us were surprised that the best control is in a county with major social and economic challenges, while some of the worst control is in some of the wealthiest and best-served areas. One possibility is that the care is not so good near the big academic medical center, but another is that folks with worse diabetes aren't even getting measured at all!
What do you think?
Ben

Many of us were surprised that the best control is in a county with major social and economic challenges, while some of the worst control is in some of the wealthiest and best-served areas. One possibility is that the care is not so good near the big academic medical center, but another is that folks with worse diabetes aren't even getting measured at all!
What do you think?
Ben
Monday, August 25, 2008
Video: Automated Use of Clinical Laboratory Results in Adults
I just found out that the Jones Lecture from last May is on the web as a video. The talk covers the issues of using laboratory data in both clinical outreach to individual patients and for public health. If you want to see it, you can find it here.
Any feedback on the talk would be very welcome.
Thanks
Ben
Any feedback on the talk would be very welcome.
Thanks
Ben
Friday, August 22, 2008
Architecture for Clinical Decision Support AND Public Health
Because of the clever way Mike Gagnon designed the Vermedx® Diabetes Information System, we got an unanticipated "twofer." In addition to supporting the robust clinical decision support activities described in this blog, it also provides a unique resource for population management beyond the practice level. The database in the middle of the whole thing can be used to provide a snapshot of the current level of care for diabetes across a wide population.
Here is the layout:

So, although we started out to get a better view of the patient's situation, we wound up with a way to see the whole population. More on this soon....
Ideas?
Ben
Here is the layout:

So, although we started out to get a better view of the patient's situation, we wound up with a way to see the whole population. More on this soon....
Ideas?
Ben
Thursday, August 21, 2008
Automated Use of Clinical Laboratory Results
I was very honored to give the Jones Lecture at Dartmouth College's Thayer School of Engineering last May. The talk covered the design and evaluation of the Vermedx® Diabetes Information System. It is now available on slideshare.
Let me know what you think of it.
Thanks
Ben
Let me know what you think of it.
Thanks
Ben
Sunday, August 17, 2008
Population Reports
One of the things that's particularly difficult for a PCP to do is keep a population view of all the patients under their care. We're able to use the Vermedx® database to generate just such a view: a roster of all the provider's diabetic patients.
The first page has a summary of the panel with statistics about how many patients are included, how many are under control, and how the panel compares to the whole database and to the best practices.

Th following pages list the patients with their latest results.
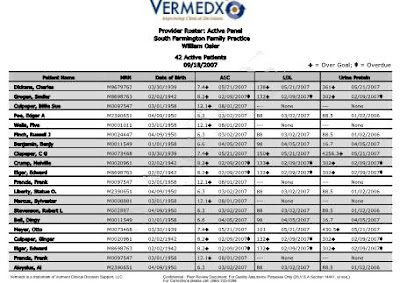
A full size version is here.
Providers can use these reports to assess their performance, monitor quality improvement efforts, and identify patients who need extra attention.
We send them out to the practices every three months. One of the nicest calls we get is "Can I have a copy of my Pop Report? I want to do some quality improvement work." That really makes my day!
The first page has a summary of the panel with statistics about how many patients are included, how many are under control, and how the panel compares to the whole database and to the best practices.

Th following pages list the patients with their latest results.
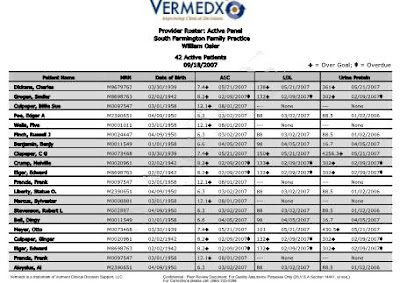
A full size version is here.
Providers can use these reports to assess their performance, monitor quality improvement efforts, and identify patients who need extra attention.
We send them out to the practices every three months. One of the nicest calls we get is "Can I have a copy of my Pop Report? I want to do some quality improvement work." That really makes my day!
Monday, August 4, 2008
Patient Reminders
After we worked out the kinks in communicating with the providers, we turned our attention to the patients. One of the big problems in diabetes care is that the patients frequently don't get their tests on time. We stimulate the practices by sending Practice Reminders when the patient is overdue for tests. We also stimulate the patient by mailing them a letter at the same time. The letter is produced by our computer, but it has the name and address of the practice and is sent on behalf of the patient's personal provider. (It can even have the logo of the sponsor such as the insurer or the practice group or a state agency.) It lists all the diabetes tests and when they are due and asks the patient to call the practice to set up testing.

A full size version is here.
These letters stimulate the patient to call the office and get back in care. They inform and activate the patient while the Practice Reminders prepare and activate the practice team, just like the Chronic Care Model says we should.
Direct outreach in this way has also turned out to be a huge patient satisfier. They just love getting these reminders and we have gotten many calls and notes from patients thanking us for the service.

A full size version is here.
These letters stimulate the patient to call the office and get back in care. They inform and activate the patient while the Practice Reminders prepare and activate the practice team, just like the Chronic Care Model says we should.
Direct outreach in this way has also turned out to be a huge patient satisfier. They just love getting these reminders and we have gotten many calls and notes from patients thanking us for the service.
Subscribe to:
Posts (Atom)